In 2024, BCEHS responded to 40,543 overdose/poisoning patient events, an average of 111 calls a day and 3,300 calls per month.
This represents a 4% decrease compared to 2023. However, monthly and daily call volumes remain high.
"Overdoses continue to happen in communities all over the province, in cities and rural areas, in every neighborhood, both inside and outside homes,” says Paramedic Public Information Officer, Brian Twaites.
In 2024, Fraser Health was the only health authority that saw an increase in overdose/poisoning patient events, at 3%. Interior Health registered the largest percentage decrease among the health authorities at 9%. Vancouver Coastal Health Authority had the highest total number of calls at 11,092 for the year.
By call volume, the top five communities in B.C. were Vancouver, followed by Surrey, Victoria, and Kelowna and Prince George. Victoria replaced Kelowna as the third highest community, registering a 5.3% increase in overdose/patient events compared to the previous year.
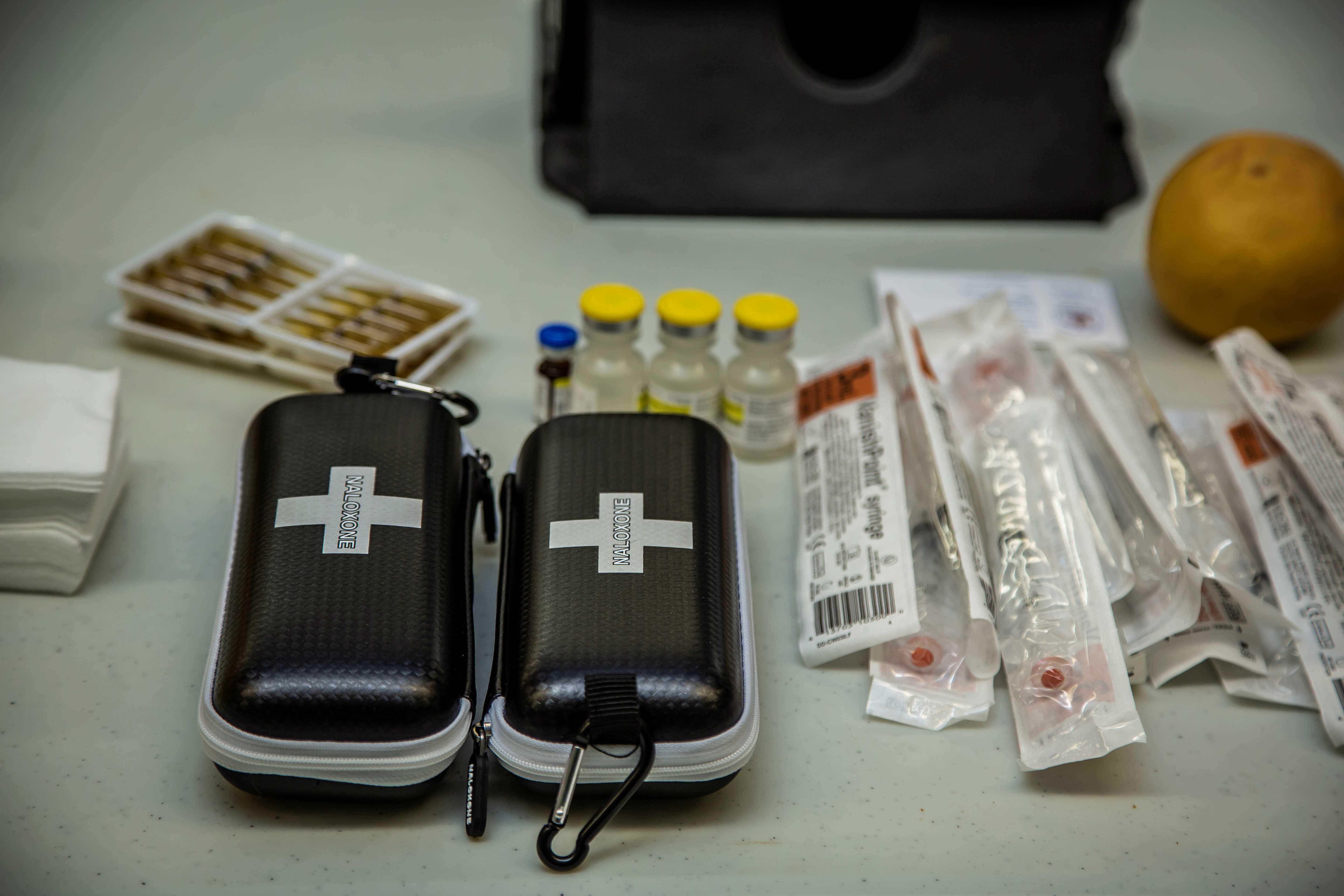
BCEHS paramedics and emergency medical call-takers have saved the lives of many drug poisoning patients. Calls related to illicit drugs are increasingly complex due to the increased toxicity of the drug supply in B.C. and BC paramedics are administering more Naloxone than ever before.
"The vast majority of illicit drug toxicity deaths happen when people use alone because there is no one to call 911," says Brian. "People need to know, if you are going to use these illicit drugs, please don't use alone.
Paramedics encourage people who use drugs to access local overdose prevention sites, available drug-checking services and have a take-home naloxone kit on hand.
"Making sure there’s someone with you and not using the same substance is the best safety net," says Brian. "If you do use alone, use the
Connect by Lifeguard app. The free app can alert 911 first responders if the user becomes unresponsive.”
People can also help by learning to recognize the signs of an overdose or drug poisoning and calling 911 when someone is unresponsive. Signs of an overdose include blue fingers or lips, shallow breathing, snoring or choking sounds, being unresponsive and not waking up.
“If you see someone that you think is unconscious, and not breathing, we want you to go and check on them,” says Brian. “Phone 911 if they are not responsive, because if they are not awake, you are the first step in that patient's survivability.”
“One of our emergency medical call takers who are trained in providing life-saving instruction will talk you through how to help the person until paramedics arrive, says Brian.
The BC Centre for Disease Control’s Take Home Naloxone (THN) program provides life-saving training and naloxone kits for free to people who are likely to witness and respond to an opioid overdose or drug poisoning, such as people who use substances, family, friends, and community members. Naloxone is a medication that quickly reverses the effects of an overdose from opioids such as heroin, methadone, fentanyl and morphine. It is available in BC without a prescription. Naloxone kits are available from community pharmacies, harm reduction sites, hospitals, First Nations sites, and correctional facilities. There are now over 2,300 sites participating across British Columbia. Visit
Toward the Heart to learn more.
In addition to saving lives, BC paramedics are connecting more drug poisoning patients to community resources through a harm reduction initiative known as ASTaR (Assess, See, Treat and Refer) Pathway which was introduced on June 1, 2022. With consent, BCEHS paramedics connect people who have experienced a drug poisoning event but do not wish to go to hospital with outreach services within their geographical region. These outreach services include but are not limited to treatment, safe supplies, housing, peer support and more. As of December 31, 2024, 754 patients were connected to services through this pathway.
“When drug poisoning patients decline to go to the hospital, paramedics have this avenue available to them to provide further care for the patients they see,” says Brian. “Anything we can do to help our patients is a step in the right direction.”
Learn More
